An anal fissure is a tear or ulcer in
the lining of the anal canal (the opening at the end of the digestive tract
where stool leaves the body).
-
- Anal fissures may occur after passage of hard or large bowel movements.
- Symptoms include pain or bleeding during ar after a bowel movement.
- The diagnosis is based on an examination of the anus.
- Treatment includes stool softeners, protective ointments, and sitz baths.
Anal fissures may be caused by an injury from a hard or large bowel movement or from frequent loose bowel movements. Uncommonly, they may also be caused by penetration of the anus during anal sex. Fissures cause the anal sphincter (the muscular ring that keeps the anus closed) to go into spasm, which worsens pain and prevents healing.
Anal fissures can occur in people of any age but are most common among infants.
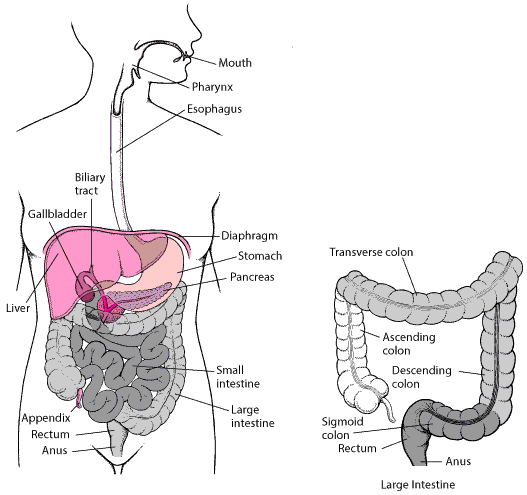
The Digestive System
Symptoms
Fissures cause pain and bleeding, usually during or shortly after a bowel movement. The pain lasts for several minutes to several hours and then subsides until the next bowel movement.

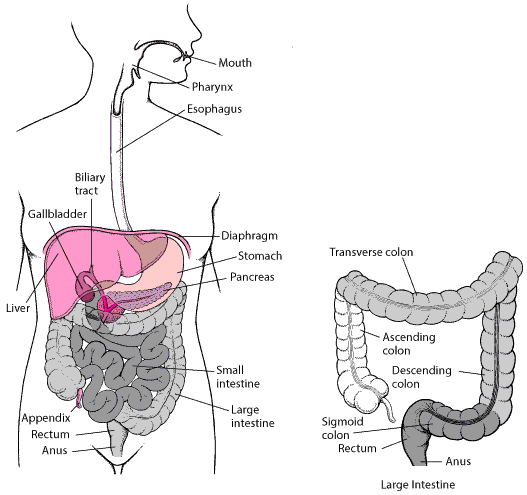
Anal Fissure
Diagnosis
A doctor diagnoses a fissure by gently inspecting the anus.
Treatment
-
- Stool softeners
- Protective ointments and sitz baths
- For anal sphincter spasms, botulinum toxin injection and nitroglycerin ointment or calcium channel blockers
A stool softener or psyllium or increased dietary fiber may reduce the possibility of injury by hard or large bowel movements. Healing is sometimes aided by using zinc oxide ointments or glycerin suppositories that lubricate the lower rectum and soften stool.
Applying topical anesthetics (such as benzocaine or lidocaine) to the anus or soaking in a warm (not hot) sitz bath for 10 to 15 minutes after each bowel movement eases discomfort and helps increase blood flow, which promotes healing. The soaking is accomplished by squatting or sitting in a partially filled tub or using a container filled with warm water placed on the toilet bowl or commode.
To reduce anal sphincter spasms and promote healing of fissures, doctors may inject the anal sphincter with botulinum toxin or have the person apply nitroglycerin ointment or calcium channel blockers (such as nifedipine cream or diltiazem gel) to the area of the fissure.
If these measures do not work, surgery may be needed. To relieve sphincter spasms, doctors cut a portion of the internal sphincter (called internal anal sphincterotomy). The anal sphincter can also be stretched (called controlled anal dilation).